RSNA Press Release
- Morbidly obese patients are vulnerable to pneumonia, infection and pulmonary embolism during surgery.
- Gastric bypass surgery carries the risk of torn sutures and stomach staple disruption in morbidly obese patients.
- Gastrointestinal surgeries to help people lose weight are expected to nearly double this year to 100,000.
Gastric Bypass Surgery Riskiest for Those Who Need It Most
Released: December 1, 2003
|
Media Contacts: |
Heather Babiar or Maureen Morley | (630) 590-7762 |
|
Heather Babiar |
Maureen Morley (630) 590-7754 mmorley@rsna.org |
CHICAGO — The same health risks that make morbidly obese patients eligible for gastric bypass surgery also leave them susceptible to complications during and after the surgery, a study of 335 patients shows.
The patients all had Roux-en-Y gastric bypass at the University Hospitals of Cleveland from 1998 to 2002. Roux-en-Y is the most popular surgery in the treatment of severely obese patients to help weight loss. It involves stapling the upper stomach to create a small pouch that is then attached to the small intestine, reducing the capacity of the stomach. Subsequent radiologic imaging helped to identify 57 complications from the surgeries — many of them multiple problems in the same patients — including suture tears and leaks, pulmonary embolism, pneumonia and infection.
"This should not be considered a cosmetic procedure," said Elmar Merkle, M.D., the lead author of the study, who presented the findings today at the 89th Scientific Assembly and Annual Meeting of the Radiological Society of North America (RSNA). "People need to be aware of the potential complications of this surgery. It basically should be the last option we can offer the morbidly obese, after other less invasive interventions such as diet and exercise have been tried."
The number of gastrointestinal surgeries for weight loss is soaring, according to the American Society for Bariatric Surgery, which estimates that the 63,000 procedures performed in 2002 will increase to 100,000 this year. Americans who are at least 100 pounds overweight are eligible for gastrointestinal surgery, according to National Institutes of Health (NIH) guidelines, but a patient who is less than 100 pounds overweight may also be considered if there is a life-threatening condition related to his or her obesity, such as type 2 diabetes or cardiopulmonary problems.
"Severely obese patients are considered to be at high risk for any type of surgery because of these co-morbidities," said Dr. Merkle, currently associate professor in the department of radiology at Duke University Medical Center in Durham, N.C. "In addition, there is a wide spectrum of procedure-specific complications following Roux-en-Y gastric bypass."
In the study, there were eight reports of anastomotic leaks and five instances of staple line disruption in the stomach, complications specific to Roux-en-Y. Three incidents of pulmonary embolism, two cases of pneumonia, and single cases of severe infection and open abdominal wound disruption were also reported — complications that are more prevalent among severely overweight patients undergoing surgery, according to Dr. Merkle.
There were also two deaths within 30 days of the 335 surgeries, but no additional deaths have been reported in the nearly 600 gastric bypass surgeries performed to date.
"Gastric bypass surgery is not about losing weight the easy way and looking good — the operation is about improving health," Dr. Merkle said. "There should be a long-term commitment by the patient. Eating habits must change. For example, patients will need lifelong vitamin supplements. Some patients lose weight, then gain it back again. Not everyone gets the results they want, but they all face the risk of these complications."
Co-authors of the study were Thomas A. Stellato, M.D., the Charles A. Hubay M.D. Professor of Surgery, founder of the bariatric program at University Hospitals of Cleveland; Cathleen Crouse, R.N., the coordinator of the bariatric program at University Hospitals; Peter T. Hallowell, M.D., who performed part of the operations; and Dean Akira Nakamoto, M.D., the director of body imaging at University Hospitals.
RSNA is an association of more than 35,000 radiologists, radiation oncologists and related scientists committed to promoting excellence in radiology through education and by fostering research, with the ultimate goal of improving patient care. The Society is based in Oak Brook, Ill.
 |
|
|
'Abscess': 43 year old woman 8 days following bariatric surgery. Computed tomography shows an abscess which contains fluid and air in the abdomen next to the gastric pouch. |
|
 |
|
|
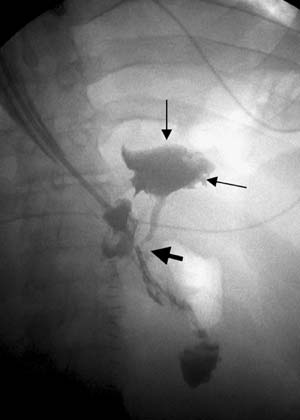
'Anastomotic leak': 18 year old man 2 days after bariatric surgery. Radiogram shows anastomotic leak (black arrow) causing contrast extravasation into the peritoneal space (thin black arrows). |
|
 |
|
|
'Acute gastric distension': 44 year old woman 4 months after bariatric surgery. Computed tomography shows severe distension of the native stomach which is caused by an internal hernia—a complication which is common following RYGB. |
|
 |
|
|
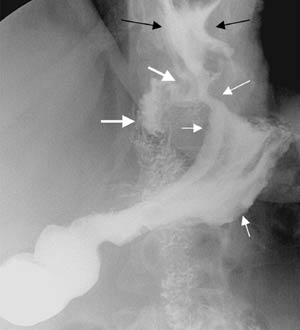
'Staple line disruption': 53 year old woman 2 months post gastric
bypass. Radiogram shows contrast passing from the gastric pouch not only
into the small bowel, but also into the native stomach. This complication
causes the |
# # #
 PDF
PDF